An Epidemiologist Separates Fact from Fiction and Offers Hope for the Future
Epidemiologists seek to learn why, how and when some people contract diseases when others don’t. Their findings are used to help monitor public health status, develop new medical treatments and disease prevention efforts, and provide an evidence base to healthcare and policy leaders.
Whether you feel the coronavirus is receding or set to surge, that testing is plentiful or inadequate, or that cases are reported as too high or too low may vary considerably based on where you live and your political leanings.
For an objective, no-spin perspective, we checked in with Jodie Guest, PhD, an epidemiologist at Emory University in Atlanta. Dr. Guest’s life’s work is studying the distribution, causes, prevention and control of diseases in populations.
Her answers to some of today’s most important questions about COVID-19 are below. Please note these reflect the situation mid-September…check our website for further updates.
Q: Are we seeing a slowdown in the number of new COVID-19 cases in the U.S.?
Dr. Guest: The number of new cases has, fortunately, plateaued or slowed down, but in many places the plateaus reflect substantially higher numbers than were reported in April, when everyone was still staying home. My concern is with schools and businesses reopening and less willingness to follow safety guidelines, the numbers may creep back up.
Q: What sites do you trust for accurate reporting on COVID-19?
Dr. Guest: I compare numbers from Johns Hopkins, Centers for Disease Control (CDC) and Worldometer to see if they match.
Q: What is the significance of the latest report from the CDC that just 6% of coronavirus deaths to date have COVID-19 as the only cause of death?
Dr. Guest: It’s not at all surprising for two reasons. One is that more than 60% of Americans have an underlying condition, such as obesity or diabetes. The risk of complications and hospitalization for people with two to three underlying conditions who contracted the virus is up to five times greater than for people with no [underlying] conditions. Second, death certificates list everything that may have contributed to mortality, including comorbid conditions and conditions caused by COVID-19 such as pneumonia. This does NOT mean that any of the more than 200,000 people who had heart disease or diabetes as an underlying condition didn’t actually die of COVID-19.
Q: Why are people of color and Latinos at greater risk of death from COVID-19?
Dr. Guest: This is not about a genetic risk of death. It’s driven by multiple factors, including a higher incidence of underlying conditions, less access to proper healthcare, greater risk of infection at the workplace and crowded living conditions that preclude social distancing.
Q: What is your take on the revised CDC guidelines that say testing for people who have been exposed to COVID-19 should be limited to those with symptoms?
Dr. Guest: Many of us in the public health community feel very strongly that we need to be testing asymptomatic people. From a public health perspective, more testing of asymptomatic people, not less, must be done to control the virus. NOTE: As of 9.18.20, CDC guidelines were revised again to state: “if you have been in close contact, such as within 6 feet of a person with documented SARS-CoV-2 infection for at least 15 minutes, and do not have symptoms, you need a test.”
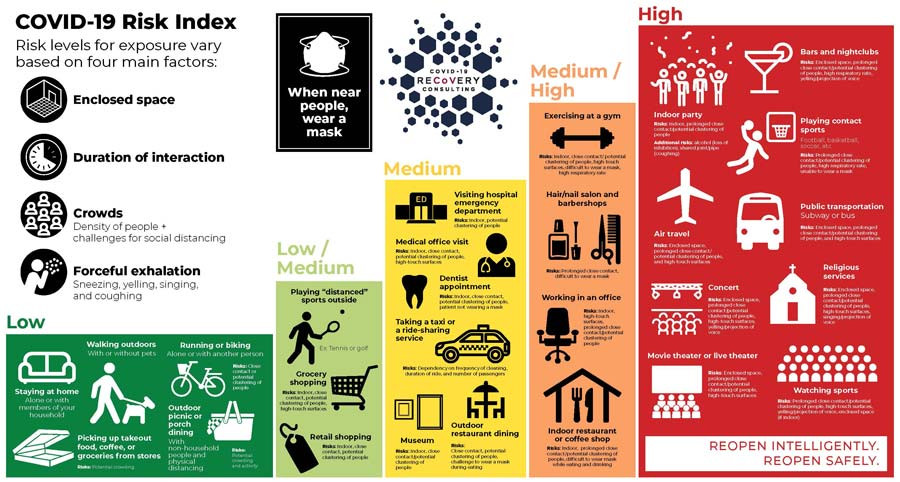
Q: What are the relative risks of activity as we move forward?
Dr. Guest: There’s so much variation based on how carefully an activity is done, but there are four good rules that apply to all: Outside is safer than inside, shorter time is safer than longer, small groups are safer than bigger, and distance is safer than closeness.
Q: How might COVID-19 affect the epidemic of flu we see annually?
Dr. Guest: If we take COVID-19 prevention measures seriously – masking, social distancing, handwashing – we could have a light flu season. If we don’t, COVID-19 will make it worse. The good news is that this has already spurred many people to get their flu shots.
Q: Any other silver linings you’re seeing?
Dr. Guest: For the first time, we are having a national conversation around health disparities and inequalities. We might actually come to a reckoning and take corrective action, and that would be spectacular.
Q: What is most important for people to know about getting back to normal?
Dr. Guest: Eventually we’ll have a vaccine but we’re not going to eliminate COVID-19 completely. However, there needn’t be this level of impact on our society. I can’t emphasize enough that we have control over how this virus spreads. We need strict guidelines and most importantly, a social contract with everyone in your community. This may be the first time many of us are asking “What are we willing to do for each other?” I hope we can all rise to the challenge.
When considering whether it is safe to resume an activity, there is much variation based on how carefully an activity is done. Additional details are provided in the infographic below, courtesy of www.covid19reopen.com
The post Can We Co-Exist with COVID-19? appeared first on Specialdocs Consultants.