This Too Shall Pass: Treating and Preventing Kidney Stones
More common, frequently less painful and far more preventable than reputed, kidney stones have, entered a new era of highly effective, noninvasive procedures. We bring you up to date on kidney stone treatment & prevention
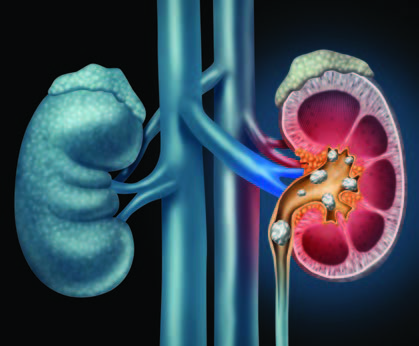
Q: Why do kidney stones happen?
A: They form when substances such as calcium, oxalate, cystine or uric acid are present at high levels in urine, becoming crystals that gradually increase in size to a stone. According to the Urology Care Foundation, Calcium stones are the most common (80%), with Uric Acid and Struvite / Infection stones making up the other 20%.
Q: How likely am I to experience kidney stones?
A: One in 10 people deal with kidney stones in their lifetime, more frequently men, but in recent years, women are rapidly closing the gap. Genetic factors also play a role: if kidney stones are prevalent among your family members, you are at higher risk of developing them.
Q: Are kidney stones very painful?
A: Over the years, the pain associated with kidney stones has taken on an almost mystical aura, sometimes described as “worse than childbirth.” However, the truth is that not every kidney stone causes intense pain. Some are small enough to pass unnoticed, and many are asymptomatic and only discovered when blood is found in the urine during routine testing. Others are large but can stay in the kidney forever without incident. It is only the stones that become “stuck” on their way out of the body that cause renal colic, or waves of severe pain, which can be promptly treated with pain medication.
Q: Does back pain mean I have kidney stones?
A: This is frequently asked by patients concerned about pain felt in the flank area near the kidney. A careful history will be taken to help determine the location of the pain, but a fairly simple way to distinguish the cause is to change positions. If the pain worsens, it is more likely to be a musculoskeletal type of strain. Kidney stone pain is less likely to be positional.
Q: How do you determine if treatment is needed?
A: A noninvasive, less expensive ultrasound is used for screening, but a spiral computed tomography (CT) scan provides superior imagery used to more accurately pinpoint the stone’s location. If only a partial obstruction is seen and not much pain is involved, time is on your side and we can wait to see if the stone passes naturally. At that point, many patients can rest comfortably at home and may be given antispasmodics (such as Flomax) to relax the ureter, pain medications to manage pain and instructed to drink plenty of water to aid the stone’s passage.
Q: What if it doesn’t pass on its own?
A: It’s reassuring to realize there is no urgency to remove the stone unless the kidney is obstructed or infected or the patient is experiencing intractable pain. And when removal is indicated, urologists (specialists in diseases of the urinary tract) have a number of options available, many of them noninvasive or minimally invasive. Open surgical procedures are a rare event. Instead, an outpatient ureteroscopy can be done, using an endoscope to break up or remove the stone. Even less invasive is lithotripsy, good for small stones, which directs high-energy shock waves toward the stone and breaks it into fragments to more easily pass out of the body. For extremely large or resistant stones, a minimally invasive percutaneous nephrolithotomy is conducted to remove the stone via an endoscope inserted through a small incision in the skin.
Q: What is the best way to prevent kidney stones from forming again?
A: We can take the time to develop an individualized approach, based on your stone’s composition. First, your stone will be tested and categorized as calcium oxalate (the most common type), calcium phosphate, a mix or a non-calcium type. Also recommended is a 24-hour urine collection to form a clear picture of how the crystals form in your body, as well as blood tests for further analysis. While those who have formed stones before are at higher risk for forming a subsequent one, we know that dietary modifications tailored to stone type and – if needed – drug therapy can substantially reduce that risk. If you form calcium oxalate stones, we’ll work on a plan to avoid foods high in oxalate, such as spinach, beets and rhubarb, and keep sodium consumption at a minimum. Also important to know is that despite its role in the stone’s composition, there is no need to restrict calcium. In fact, increasing your calcium intake with higher-calcium foods such as milk, yogurt and cheese can help lower oxalate levels in the urine. Finally, keep in mind that the single best preventive measure is to simply fill a bottle with water and drink often.
The post Kidney Stones: Treatment & Prevention appeared first on Specialdocs Consultants.
